News
ALL NEWSResearch
December 15, 2022
Tracking plasma cell survival (Ise G, in J. Exp. Med.)
Researchers led by Osaka University use a novel tracing method to track the survival of antibody-producing plasma cells
Just as a fire department mobilizes in response to a reported fire, specialized immune cells in the body mobilize in response to the introduction of foreign substances known as antigens. Plasma cells are an important type of immune cell that release antibodies (or protective proteins) that act to neutralize antigens. Recently, researchers from Japan have shed new light on the survival of plasma cells in the body.
In a recent study published in Journal of Experimental Medicine, researchers led by Osaka University have employed a novel experimental system to trace the development and longevity of plasma cells over time.
Plasma cells are generated by the spleen and lymphoid organs in response to antigen exposure. Many plasma cells die shortly after participating in an immune response, but a small population of plasma cells called long-lived plasma cells (LLPCs) can survive in the body for months or even years. The researchers sought to explore the dynamics of this LLPC population to better understand how antibody-mediated immunity is maintained in the body.
“Our goal was to track the long-term survival of plasma cells,” says lead author of the study Takuya Koike. “To this end, we designed a mouse model in which plasma cells in the spleen and bone marrow were labeled by a fluorescent reporter in response to a specific drug treatment.”
The researchers monitored the survival of fluorescently labeled plasma cells in the spleen, bone marrow, and gut for over a year and found that the frequency of fluorescent plasma cells decreased to less than 60% within 1 month, and as low as 3%–20% within 1 year. The bone marrow appeared to contain more fluorescent plasma cells at one year than the spleen or gut, indicating that LLPCs may preferentially reside in bone marrow niches.
“Our results indicated that the plasma cell population likely experiences frequent turnover, with new plasma cells replenishing the cells that are lost over time, while only a small portion of cells differentiates into LLPCs,” explains senior author Wataru Ise. Analysis of another mouse model in which only newly generated plasma cells were labeled allowed the researchers to identify specific molecular markers that can distinguish LLPCs from short-lived plasma cells.
These findings provide deeper insights into the longevity of plasma cells. Better understanding of the LLPC population may aid in the development of new vaccines that efficiently induce the generation of LLPCs, thereby strengthening the body’s antibody-mediated immune response.
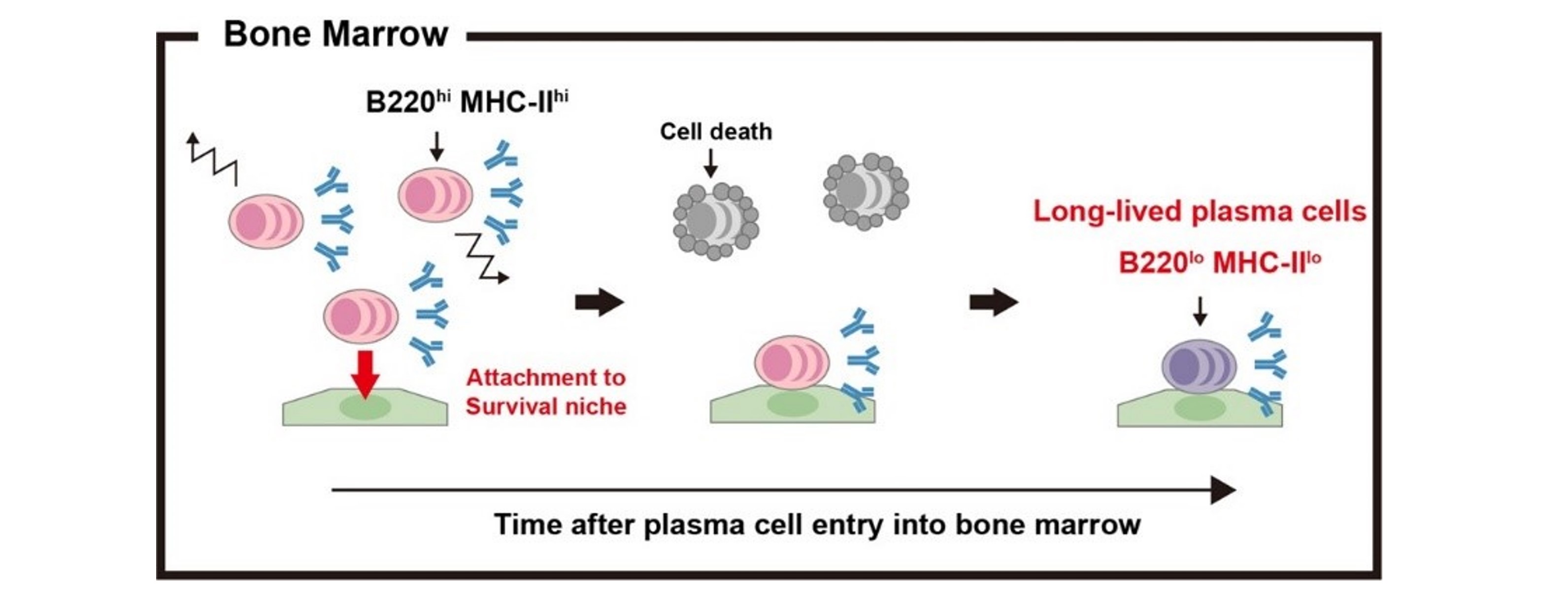
Fig. 1
Most of plasma cells that arrive at bone marrow are short-lived B220(hi) MHC-II(hi) cells. A small fraction of them become immobilized to bone marrow niches and progressively differentiate into long-lived B220(lo) MHC-II(lo) cells.
License: Original content
Usage restriction: Cannot be used without permission.
Credit: Koike et al.
Online signing ceremony on April 22, 2022
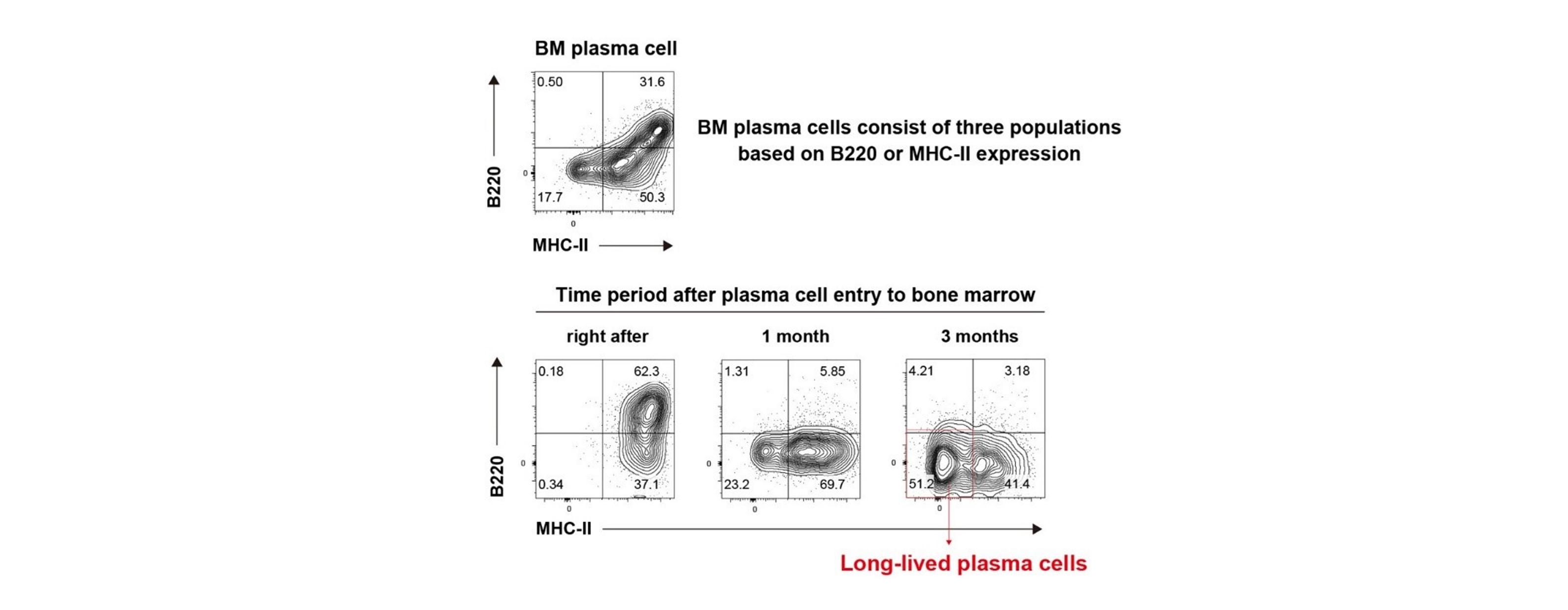
Fig. 2
Plasma cells right after arriving at bone marrow are B220(hi) MHC-II(hi), whereas those survived for long period of time in bone marrow become B220(lo) MHC-II(lo).
License: Original content
Usage restriction: Cannot be used without permission.
Credit: Koike et al.
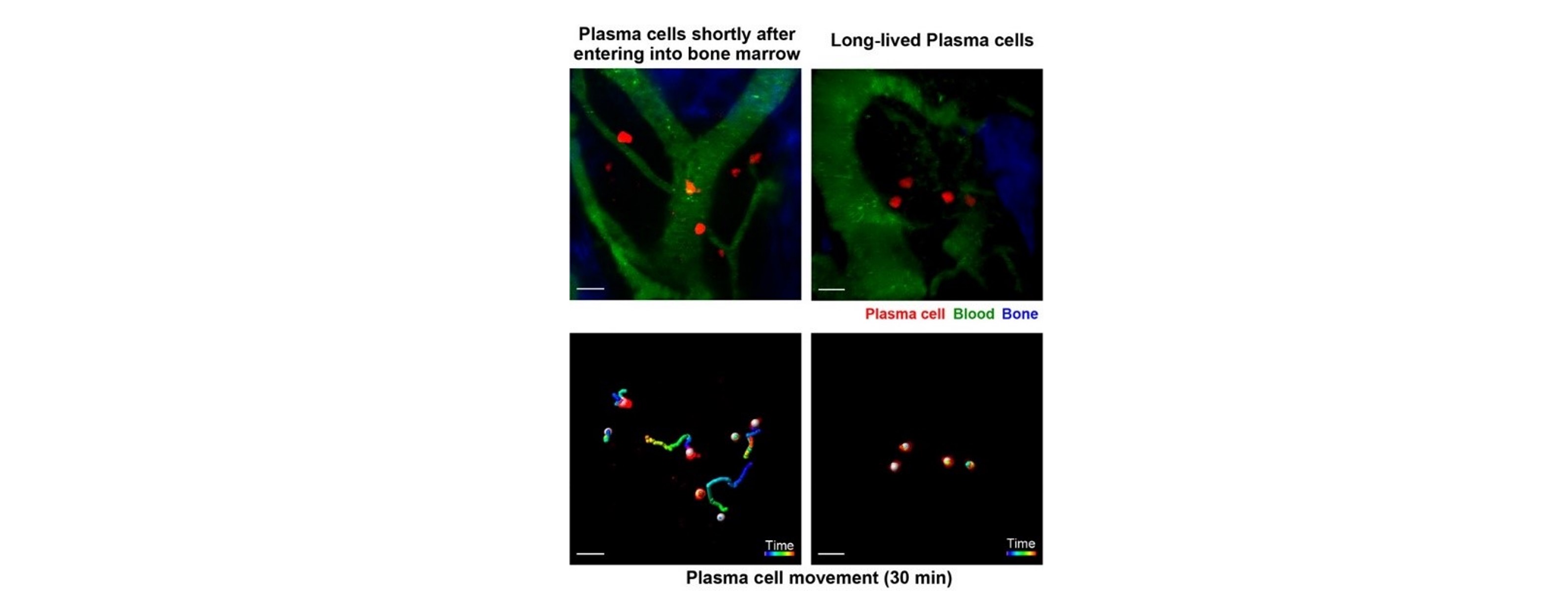
Fig. 3
Plasma cells right after arriving at bone marrow are motile and migratory, whereas long-lived plasma cells are sessile and immobilized in the bone marrow environment.
License: Original content
Usage restriction: Cannot be used without permission.
Credit: Koike et al.
The article,“Progressive differentiation towards the long-lived plasma cell compartment in the bone marrow,” was published in Journal of Experimental Medicine
Title: Progressive differentiation towards the long-lived plasma cell compartment in the bone marrow
Journal: Journal of Experimental Medicine
Authors: Takuya Koike, Kentaro Fujii, Kohei Kometani, Noah S. Butler, Kenji Funakoshi, Shinya Yari, Junichi Kikuta, Masaru Ishii, Tomohiro Kurosaki and Wataru Ise
DOI: https://doi.org/10.1084/jem.20221717
Funded by:
Nippon Foundation
Otsuka Pharmaceutical Co., Ltd.
Grant-in-Aid for JSPS Fellows
Grant-in-Aid for Young Scientists
JSPS KAKENHI
the SENSHIN Medical Research Foundation
the Uehara Memorial Foundation
the Naito Foundation
Daiichi Sankyo Foundation of Life Science.